Ventricular Tachycardia
Definition | Aetiology | Pathophysiology | Risk Factors | Signs and Symptoms | Investigations | Management | Patient Advice
Definition
Ventricular Tachycardia (VT) is a life-threatening arrhythmia originating in the ventricles, characterised by a fast heart rate (≥100 beats per minute) with three or more consecutive ventricular beats. See Figure 1.
Aetiology
Causes of VT include:
- Ischaemic Heart Disease: Commonly occurs post-myocardial infarction due to scarring in the heart muscle.
- Cardiomyopathies: Conditions like dilated or hypertrophic cardiomyopathy.
- Electrolyte Abnormalities: Low potassium or magnesium levels.
- Drug Toxicity: E.g., digoxin toxicity or use of antiarrhythmics.
- Genetic Conditions: E.g., Long QT syndrome or Brugada syndrome.
Pathophysiology
VT occurs due to abnormal electrical activity in the ventricles:
- Re-entry Circuits: Electrical signals re-enter damaged areas, causing repetitive ventricular activation.
- Enhanced Automaticity: Increased spontaneous electrical activity in ventricular cells.
- Trigger Activity: Abnormal electrical signals triggered by afterdepolarisations.
Risk Factors
Factors increasing the risk of VT include:
- Previous myocardial infarction.
- Heart failure or reduced left ventricular ejection fraction (LVEF).
- Electrolyte disturbances, e.g., low potassium or magnesium.
- Family history of genetic arrhythmia syndromes.
- Use of QT-prolonging medications.
Signs and Symptoms
Symptoms of VT include:
- Palpitations: Sensation of rapid or irregular heartbeats.
- Dizziness: Caused by reduced cardiac output.
- Syncope: Sudden loss of consciousness due to inadequate blood flow to the brain.
- Chest Pain: Due to reduced oxygen supply to the heart muscle.
- Shortness of Breath: Due to decreased cardiac efficiency.
Investigations
Tests to diagnose VT include:
- 12-Lead ECG:
- Shows wide QRS complexes (>120 ms) and a fast ventricular rate.
- Fusion or capture beats may indicate VT rather than supraventricular tachycardia (SVT).
- Blood Tests:
- Electrolytes: Check potassium, magnesium, and calcium levels.
- Cardiac Markers: Elevated troponins may indicate myocardial ischaemia.
- Echocardiography: Assesses ventricular function and identifies structural abnormalities.
- Cardiac MRI: Evaluates scarring or fibrosis in the myocardium.
- Electrophysiological Study (EPS): Maps abnormal electrical pathways and identifies re-entry circuits.
Management
1. Acute Management
- Unstable VT: Immediate synchronised electrical cardioversion.
- Stable VT: Antiarrhythmic medications such as amiodarone (300 mg IV loading dose, then 900 mg over 24 hours).
2. Long-Term Management
- Implantable Cardioverter-Defibrillator (ICD): Device implanted to detect and treat VT episodes automatically.
- Catheter Ablation: Procedure to destroy re-entry circuits in cases of recurrent or refractory VT.
- Medication: Beta-blockers (e.g., bisoprolol) or antiarrhythmics (e.g., sotalol) to prevent recurrences.
3. Specialist Referral
Referral to cardiology is essential for:
- Assessment for ICD implantation.
- Evaluation for underlying causes, including ischaemia or cardiomyopathy.
Patient Advice
Key advice includes:
- Avoid triggers such as stress, stimulants, and QT-prolonging medications.
- Take medications as prescribed to prevent recurrence.
- Maintain regular follow-up appointments to monitor heart health and device function if an ICD is implanted.
- Seek urgent medical attention if symptoms like chest pain, syncope, or palpitations recur.
Figure 1
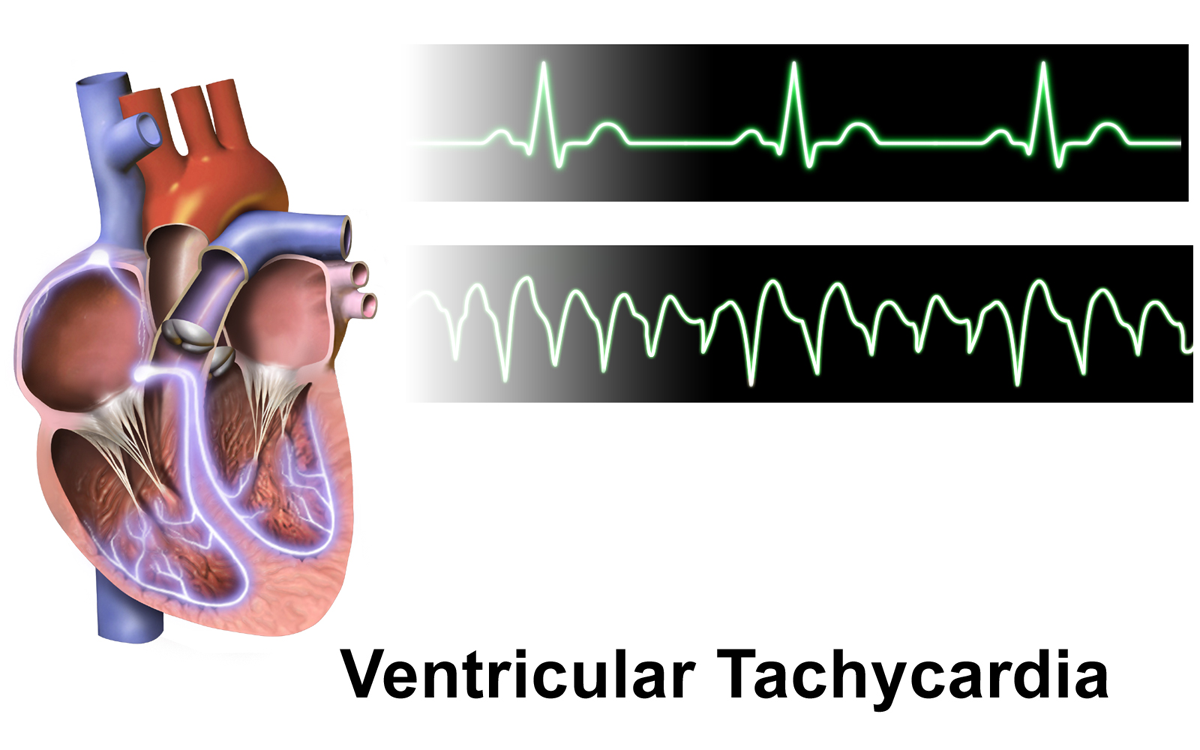
Image showing an ECG example of ventricular tachycardia.
References
- BruceBlaus (2015). Ventricular Tachycardia [Image]. Available at: https://upload.wikimedia.org/wikipedia/commons/d/d4/Ventricular_Tachycardia.png (Accessed: 30 December 2024).
Check out our youtube channel
Blueprint Page
Explore the comprehensive blueprint for Physician Associates, covering all essential topics and resources.
Book Your Session
Enhance your skills with personalised tutoring sessions tailored for Physician Associates.

