Varicose Veins
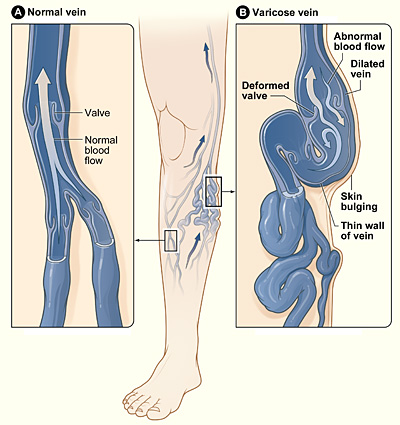
Image: Varicose veins as seen in the legs. Image by Drahreg01, available under the Creative Commons Attribution-Share Alike 4.0 International license.
Definition | Aetiology | Pathophysiology | Risk Factors | Signs and Symptoms | Investigations | Management
Definition
Varicose veins are enlarged and twisted veins, typically in the legs, caused by malfunctioning valves within the veins. These valves normally help to keep blood flowing in the correct direction, but when they become weakened or damaged, blood can flow backwards and pool in the vein. This causes the vein to enlarge and twist, leading to symptoms such as swelling, pain, and aching. In some cases, varicose veins can also lead to more serious complications such as blood clots or skin ulcers.
Aetiology
Varicose veins are caused by a malfunction in the valves of the veins, usually in the legs. These valves are responsible for keeping blood flowing in the correct direction (towards the heart), but if they become weakened or damaged, blood can begin to flow in the wrong direction and pool in the veins. This can cause the veins to become enlarged and twisted, leading to the characteristic appearance of varicose veins.
Pathophysiology
Varicose veins occur when the valves in the veins, responsible for keeping blood flowing towards the heart, become weakened or damaged. This allows blood to flow in the wrong direction and pool in the veins, causing them to become enlarged and twisted. The increased pressure in the veins can cause the walls of the veins to stretch, leading to the characteristic appearance of varicose veins. This increased pressure can also cause blood to leak out of the veins into the surrounding tissue, leading to inflammation and pain. In some cases, varicose veins can also lead to the development of blood clots or ulcers.
Risk Factors
There are several risk factors for developing varicose veins, including:
- Heredity: A family history of varicose veins increases the likelihood of developing them.
- Pregnancy: Pregnant women are at increased risk due to the added pressure on the veins in the legs from the growing uterus.
- Obesity: Excess weight can put extra pressure on the veins in the legs, increasing the risk of varicose veins.
- Prolonged standing or sitting: People who stand or sit for long periods, such as those in jobs that require them to be on their feet all day, are at increased risk.
- Age: The risk of varicose veins increases with age.
- Hormonal changes: Menopause, hormone replacement therapy, and birth control pills can also increase the risk.
- Trauma or injury to the legs: Injury to the legs can damage veins, leading to varicose veins.
- History of blood clots or thrombosis: Previous clots can damage veins, increasing the risk of varicose veins.
- Smoking: Smoking can damage blood vessels and contribute to varicose veins.
- Lack of physical activity: A sedentary lifestyle increases the risk of developing varicose veins.
Signs and Symptoms
The signs and symptoms of varicose veins include:
- Visible, swollen veins: Typically on the legs, often blue or dark purple in colour.
- Aching or heavy feeling in the legs: Especially after standing or sitting for long periods.
- Itching or burning sensation: Around the affected veins.
- Swelling in the legs or ankles: Common in more severe cases.
- Cramping or muscle fatigue: Particularly in the legs.
- Restless legs: A common symptom, particularly at night.
- Dry or thickened skin: Over the affected veins.
- Discolouration or pigmentation changes: Around the affected veins.
- Skin ulcers: Typically around the ankle area, a more severe complication.
- Varicose eczema: An itchy, red, dry, and scaly rash near the varicose veins.
Investigations
Doppler ultrasound: A non-invasive test using sound waves to create images of blood flow in the veins, helping to identify any blood clots or blockages.
Management
Several treatment options are available for varicose veins, including:
- Compression stockings: Tight-fitting stockings that apply pressure to the legs, improving blood flow and reducing swelling. Often recommended as a first-line treatment for mild to moderate varicose veins.
- Lifestyle changes: Regular exercise, maintaining a healthy weight, and avoiding prolonged standing or sitting can help reduce symptoms.
- Simple analgesia: Pain relief for discomfort associated with varicose veins.
- Referral to vascular specialists: In cases where symptoms are severe, or complications arise, a referral to a vascular specialist may be necessary. Surgical options may be considered, including procedures like sclerotherapy, endovenous laser treatment, or vein stripping.
References
- NHS (2024) Varicose Veins. Available at: https://www.nhs.uk/conditions/varicose-veins (Accessed: 26 August 2024).
- National Institute for Health and Care Excellence (NICE) (2024) Varicose Veins: Diagnosis and Management. Available at: https://www.nice.org.uk/guidance/cg168 (Accessed: 26 August 2024).
Previous Topic (Arterial Occlusion)
Next Topic (Aortic aneurysm)
Check out our youtube channel
Blueprint Page
Explore the comprehensive blueprint for Physician Associates, covering all essential topics and resources.
Book Your Session
Enhance your skills with personalised tutoring sessions tailored for Physician Associates.

