Temporal Arteritis (Giant Cell Arteritis)
Definition
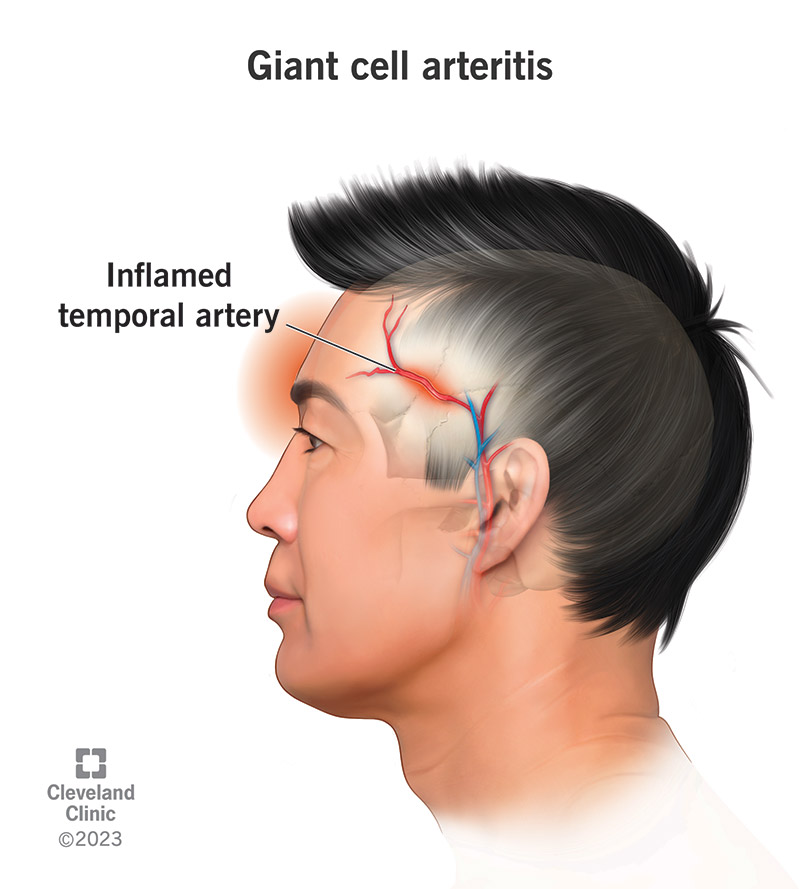
Temporal arteritis, also known as giant cell arteritis (GCA), is a form of vasculitis that causes inflammation of the large and medium-sized arteries. It primarily affects the arteries in the head, especially the temporal arteries. If left untreated, it can lead to serious complications such as vision loss or stroke.
Aetiology
The exact cause of temporal arteritis is unknown. It is believed to be an autoimmune condition where the immune system mistakenly attacks the arterial walls. Genetic and environmental factors may play a role in its development.
Pathophysiology
In temporal arteritis, the inflammation of the arterial walls leads to thickening and swelling, which narrows the arteries and reduces blood flow. This can cause ischaemia in the affected tissues. The inflammation is typically granulomatous, involving giant cells, hence the name "giant cell arteritis."
Risk factors
- Age (most common in people over 50)
- Female gender
- Scandinavian or Northern European descent
- Polymyalgia rheumatica
- Family history of giant cell arteritis
Signs and Symptoms
- New-onset headache, typically in the temporal region
- Scalp tenderness
- Jaw claudication (pain in the jaw muscles when chewing)
- Visual disturbances (e.g., blurred vision, double vision, sudden vision loss)
- Fatigue and malaise
- Fever
- Weight loss
Red Flags
- Sudden vision loss
- Stroke symptoms (e.g., weakness, slurred speech)
- Severe headache with fever
- Severe jaw pain
Investigations
- Clinical history and physical examination, focusing on temporal artery tenderness and thickening
- Blood tests: Elevated erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP)
- Temporal artery biopsy: Gold standard for diagnosis, showing inflammation and giant cells in the artery walls
- Ultrasound of the temporal arteries: May show a halo sign indicative of inflammation
- MRI or CT angiography if large vessel involvement is suspected
Management
Primary Care Management:
- Immediate initiation of high-dose corticosteroids (e.g., prednisolone 40-60 mg daily) if GCA is suspected, to prevent vision loss
- Referral to a specialist (e.g., rheumatologist) for further evaluation and management
- Monitoring for side effects of corticosteroids, such as osteoporosis and diabetes
- Adjunctive therapy with aspirin to reduce the risk of ischaemic complications
Specialist Management:
- Long-term corticosteroid therapy with gradual tapering based on clinical response and inflammatory markers
- Consideration of steroid-sparing agents (e.g., methotrexate) for patients with relapsing disease or those at high risk of corticosteroid side effects
- Tocilizumab (an IL-6 receptor antagonist) for refractory or relapsing GCA
- Regular follow-up to monitor disease activity and treatment side effects
Example Management for Temporal Arteritis:
A patient presenting with symptoms suggestive of temporal arteritis should be started on high-dose prednisolone (40-60 mg daily) immediately to prevent vision loss, even before the diagnosis is confirmed. They should be referred to a rheumatologist for further management. Once the diagnosis is confirmed, corticosteroid therapy is continued with gradual tapering based on clinical response and inflammatory markers. Adjunctive therapy with aspirin may be considered to reduce the risk of ischaemic complications. If the disease is relapsing or if there are significant side effects from corticosteroids, additional immunosuppressive therapy, such as methotrexate or tocilizumab, may be used.
References:
- NICE. (2023). Giant Cell Arteritis: Diagnosis and Management. Retrieved from https://cks.nice.org.uk/topics/giant-cell-arteritis/diagnosis/suspecting-giant-cell-arteritis/
- NICE. (2023). Giant Cell Arteritis: Management. Retrieved from https://cks.nice.org.uk/topics/giant-cell-arteritis/management/management/
- NHS. (2023). Giant Cell Arteritis (Temporal Arteritis). Retrieved from https://www.nhs.uk/conditions/giant-cell-arteritis/
- Ropper, A. H., & Samuels, M. A. (2019). Adams and Victor's Principles of Neurology. 11th ed. McGraw-Hill Education.
- O'Sullivan, S. B., & Schmitz, T. J. (2016). Physical Rehabilitation. 6th ed. F.A. Davis Company.
Check out our youtube channel
Blueprint Page
Explore the comprehensive blueprint for Physician Associates, covering all essential topics and resources.
Book Your Session
Enhance your skills with personalised tutoring sessions tailored for Physician Associates.



