Phimosis and Paraphimosis
Definition | Aetiology | Pathophysiology | Risk Factors | Signs and Symptoms | Investigations | Management | Example Management | References
Definition
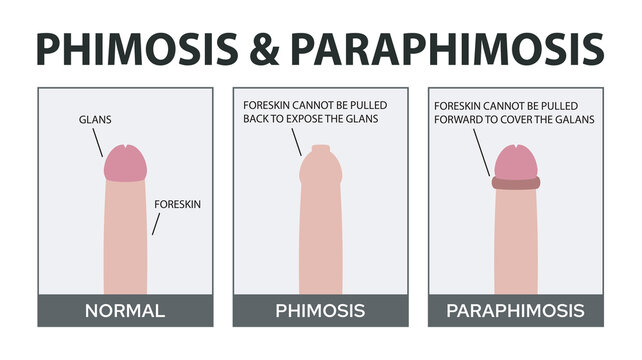
Phimosis and paraphimosis are conditions affecting the foreskin of the penis. Phimosis is the inability to retract the foreskin over the glans penis. Paraphimosis occurs when the retracted foreskin cannot be returned to its normal position, leading to a tight band around the glans and potentially compromising blood flow.
Aetiology
Phimosis and paraphimosis can result from various causes:
- Congenital phimosis: A normal condition in infants and young children where the foreskin is naturally tight.
- Pathological phimosis: Often due to scarring from infections (e.g., balanitis), trauma, or chronic inflammation.
- Paraphimosis: Typically caused by improper retraction of the foreskin, often during catheterisation, cleaning, or sexual activity.
Pathophysiology
In phimosis, the tight foreskin restricts retraction over the glans, which can cause difficulties with hygiene, urination, and sexual function. Paraphimosis occurs when the retracted foreskin forms a constricting band behind the glans, leading to venous and lymphatic obstruction. This can cause swelling and pain and, if untreated, can result in arterial compromise and necrosis of the glans.
Risk Factors
- Age: Phimosis is common in young boys but usually resolves by adolescence.
- Infections: Recurrent balanitis or balanoposthitis.
- Trauma: Injury to the foreskin or glans.
- Poor hygiene: Leading to infections and scarring.
- Catheterisation: Incorrect technique can lead to paraphimosis.
Signs and Symptoms
- Phimosis: Inability to retract the foreskin, pain during urination, ballooning of the foreskin during urination, recurrent infections.
- Paraphimosis: Pain and swelling of the glans, constricting band of tissue behind the glans, inability to move the foreskin over the glans, possible signs of ischaemia (discolouration of the glans).
Investigations
- Clinical history and physical examination.
- Assessment of symptoms and any associated infections or trauma.
- Ultrasound: In rare cases, to assess blood flow in suspected ischaemia.
Management
Primary Care Management
- If the patient is unwell, refer urgently to hospital and then stabilise the patient, ensuring airway, breathing, and circulation (ABCs).
- Topical steroid creams: For phimosis, apply betamethasone 0.05% cream twice daily for 4-8 weeks to reduce inflammation and allow retraction.
- Gentle manual retraction: Encouraged for boys with non-pathological phimosis.
- Patient education: Emphasise good hygiene practices and the importance of not forcibly retracting the foreskin in young children.
- For paraphimosis: Attempt manual reduction by applying gentle pressure to the glans while pushing the foreskin forward. Ice packs or sugar solutions can be used to reduce swelling before reduction.
- Referral to a specialist (urologist) if manual reduction fails, for further management.
Specialist Management
- Surgical intervention: Circumcision or preputioplasty for recurrent or severe phimosis.
- Dorsal slit procedure: Emergency procedure for irreducible paraphimosis to relieve constriction.
- Treatment of underlying conditions: Address infections or other contributing factors.
- Post-operative care: Instructions on hygiene and care following surgical procedures.
Example Management for Phimosis and Paraphimosis
A patient presenting with phimosis can be managed with topical steroid cream, such as betamethasone 0.05% applied twice daily for 4-8 weeks. Gentle manual retraction should be encouraged, and good hygiene practices should be emphasised. For a patient with paraphimosis, manual reduction should be attempted using ice packs or sugar solutions to reduce swelling, followed by gentle pressure to move the foreskin forward. If manual reduction is unsuccessful, referral to a urologist is necessary for possible surgical intervention. Regular follow-up is essential to monitor response to treatment and manage any complications.
References
- NICE. (2024). Phimosis and Paraphimosis: Diagnosis and Management. Retrieved from NICE
- NHS. (2023). Phimosis and Paraphimosis. Retrieved from NHS
- British Association of Urological Surgeons (BAUS). (2022). Phimosis and Paraphimosis. Retrieved from BAUS
- McGregor, T. B., Pike, J. G., & Leonard, M. P. (2007). Pathologic and physiologic phimosis: Approach to the phimotic foreskin. Canadian Family Physician.
Check out our youtube channel

