Peroneal Nerve Injury (Foot Drop)
Definition
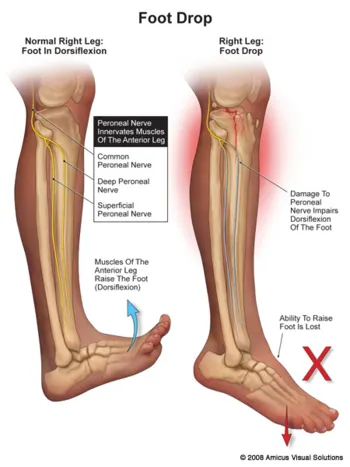
Peroneal nerve injury, commonly known as foot drop, occurs when the peroneal nerve, which controls movement and sensation in the lower leg and foot, is damaged. This injury results in difficulty lifting the front part of the foot (dorsiflexion), causing a characteristic "foot drop" gait.
Aetiology
Peroneal nerve injury can be caused by various factors, including:
- Trauma: Fractures of the fibula, knee dislocations, or penetrating injuries
- Compression: Prolonged pressure on the nerve (e.g., from leg crossing, tight plaster casts)
- Infections: Herpes zoster (shingles)
- Systemic diseases: Diabetes, rheumatoid arthritis
- Intoxication: Alcoholism or drug overdose leading to prolonged pressure on the nerve
- Surgical complications: Hip or knee surgery
Pathophysiology
The peroneal nerve controls the muscles that lift the foot and toes. Damage to this nerve disrupts the transmission of signals from the brain to these muscles, resulting in weakness or paralysis and sensory loss in the front and side of the lower leg and foot.
Risk Factors
- Trauma or injury to the leg or knee
- Prolonged immobility or improper positioning during sleep or surgery
- Systemic conditions like diabetes or rheumatoid arthritis
- Alcoholism or substance abuse
- Previous surgery around the knee or hip
Signs and Symptoms
- Inability to lift the front part of the foot (foot drop)
- Weakness in the foot and toes
- Numbness or tingling in the top of the foot and outer part of the lower leg
- Loss of sensation in the peroneal nerve distribution area
- Slapping gait (foot slaps down onto the floor with each step)
Red Flags
- Rapid progression of symptoms
- Severe pain unresponsive to standard measures
- Signs of systemic illness (e.g., fever, weight loss)
- History of cancer or recent significant trauma
- Loss of bowel or bladder function
Investigations
- Clinical history and physical examination
- Nerve conduction studies to assess the function of the peroneal nerve
- Electromyography (EMG) to evaluate muscle activity and nerve conduction
- Imaging studies (e.g., X-ray, MRI) to identify fractures or other structural causes
- Blood tests to rule out systemic conditions
Management
Primary Care Management
- Initial assessment and diagnosis based on clinical history and physical examination
- Immobilisation of the affected limb to prevent further injury
- Pain management with analgesics
- Referral to a specialist for further evaluation and treatment
Specialist Management
- Advanced diagnostic testing (e.g., nerve conduction studies, EMG)
- Physical therapy to maintain muscle strength and prevent contractures
- Occupational therapy to improve foot function and adapt daily activities
- Surgical intervention in severe cases (e.g., nerve decompression, repair, or grafting)
- Management of underlying conditions (e.g., diabetes, rheumatoid arthritis)
Example Management for Peroneal Nerve Injury (Foot Drop)
A patient presenting with foot drop due to a peroneal nerve injury following a fibula fracture should initially be managed with immobilisation of the leg in a splint and pain relief with NSAIDs. Referral to a specialist for nerve conduction studies and EMG should be arranged to assess the extent of the injury. Physical therapy should be initiated to maintain muscle strength and prevent contractures. If there is no improvement after conservative management, surgical intervention may be considered.
References
- NICE. (2024). Peripheral Neuropathy: Diagnosis and Management. Retrieved from NICE
- NHS. (2023). Peripheral Nerve Injury. Retrieved from NHS
- Campbell, W. W. (2013). Evaluation and Management of Peripheral Nerve Injury. Clinical Neurophysiology.
- Watson, J. C., & Dyck, P. J. (2015). Peripheral Neuropathy: A Practical Approach to Diagnosis and Management. Mayo Clinic Proceedings.
- Preston, D. C., & Shapiro, B. E. (2012). Electromyography and Neuromuscular Disorders: Clinical-Electrophysiologic-Ultrasound Correlations. Elsevier.
















