Image: "Patent Ductus Arteriosus" by Blausen.com staff (2014). "Medical gallery of Blausen Medical 2014". WikiJournal of Medicine 1 (2). DOI:10.15347/wjm/2014.010. ISSN 2002-4436. Licensed under CC BY 3.0. Link to the source.
Patent Ductus Arteriosus (PDA)
Definition | Aetiology | Pathophysiology | Risk Factors | Signs and Symptoms | Investigations | Management | Patient Advice
Definition
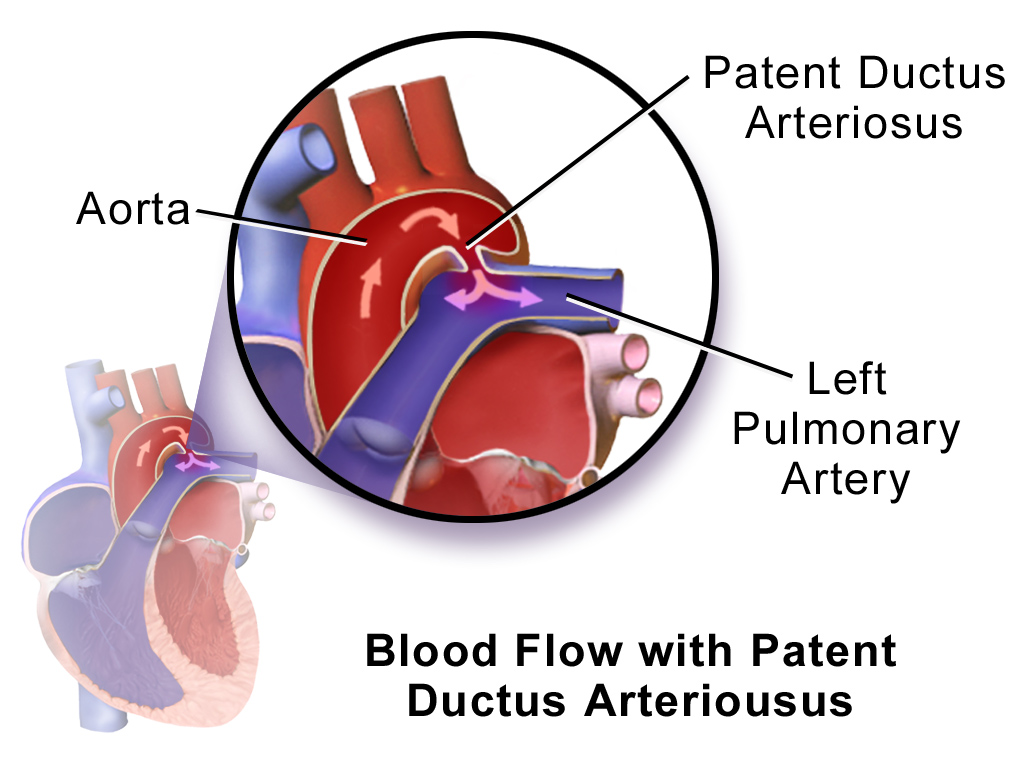
Patent Ductus Arteriosus (PDA) is a congenital heart defect where the ductus arteriosus, a fetal blood vessel that connects the pulmonary artery to the descending aorta, fails to close after birth. This results in abnormal blood flow between the aorta and pulmonary artery.
Aetiology
PDA occurs due to the failure of the ductus arteriosus to close naturally after birth. Causes include:
- Prematurity: Immature lungs fail to produce enough prostaglandin metabolism for closure.
- Congenital Rubella Syndrome: Associated with maternal rubella infection during pregnancy.
- High Altitudes: Reduced oxygen levels may delay closure.
- Genetic Syndromes: E.g., Trisomy 21 (Down syndrome).
Pathophysiology
Key processes in PDA include:
- Left-to-Right Shunting: Blood flows from the high-pressure aorta to the low-pressure pulmonary artery.
- Increased Pulmonary Blood Flow: Overload leads to pulmonary hypertension and increased workload on the left heart.
- Heart Failure Risk: Persistent overload can lead to left ventricular dysfunction.
Risk Factors
Risk factors include:
- Premature birth.
- Low birth weight.
- Female sex (more common in females).
- Maternal rubella infection during pregnancy.
- Genetic syndromes (e.g., Trisomy 21).
Signs and Symptoms
Clinical features depend on the size of the PDA and may include:
- Heart Murmur: Continuous "machinery-like" murmur heard best at the left infraclavicular region.
- Tachypnoea: Fast breathing due to pulmonary congestion.
- Failure to Thrive: Poor feeding and weight gain in infants.
- Fatigue: Particularly during feeding or physical activity.
- Recurrent Respiratory Infections: Due to pulmonary congestion.
Investigations
Diagnostic tests and findings include:
- Clinical Examination: Detects continuous murmur and bounding peripheral pulses.
- Chest X-ray: Shows cardiomegaly and increased pulmonary vascular markings.
- Echocardiography: Diagnostic test of choice:
- Demonstrates left-to-right shunting.
- Measures the size of the PDA and assesses cardiac function.
- Doppler Ultrasound: Confirms abnormal blood flow through the PDA.
- Electrocardiogram (ECG): May show left ventricular hypertrophy.
Management
1. Medical Management
- Prostaglandin Inhibitors: E.g., ibuprofen or indomethacin to facilitate ductal closure in preterm infants.
- Diuretics: E.g., furosemide for symptomatic relief of pulmonary congestion.
- Supportive Care: Optimisation of feeding and oxygenation in premature infants.
2. Surgical and Interventional Management
- Transcatheter Device Closure: Preferred in older children and adults. A catheter is used to place a closure device into the PDA.
- Surgical Ligation: Open surgical approach to tie off the PDA, often used in neonates or when device closure is not feasible.
3. Specialist Referral
Referral to a paediatric cardiologist is essential for assessment and management planning. Neonatal referral is crucial in symptomatic premature infants.
Patient Advice
Key advice includes:
- Attend regular follow-up appointments with a cardiologist.
- Ensure adequate nutrition and monitor growth in infants.
- Report symptoms such as increased breathlessness, feeding difficulties, or infections immediately.
- Parents should receive education about the condition and its management.
Check out our youtube channel
Blueprint Page
Explore the comprehensive blueprint for Physician Associates, covering all essential topics and resources.
Book Your Session
Enhance your skills with personalised tutoring sessions tailored for Physician Associates.

