Image reference: GNC Dubai
Myasthenia Gravis
Definition | Aetiology | Pathophysiology | Risk Factors | Signs and Symptoms | Investigations | Management | Example Management | References
Definition
Myasthenia Gravis (MG) is a chronic autoimmune neuromuscular disorder characterised by weakness and rapid fatigue of the voluntary muscles. The condition is caused by an interruption in the communication between nerves and muscles, leading to muscle weakness.
Aetiology
Myasthenia Gravis is caused by an autoimmune response where antibodies block or destroy nicotinic acetylcholine receptors at the neuromuscular junction:
- Autoantibodies: Against acetylcholine receptors (AChR) or muscle-specific kinase (MuSK).
- Thymus gland abnormalities: Thymomas or hyperplasia can contribute to the autoimmune response.
Pathophysiology
The autoimmune response in Myasthenia Gravis interferes with the transmission of nerve impulses to muscles. Normally, acetylcholine (ACh) released from nerve endings binds to ACh receptors on muscle cells to stimulate muscle contraction. In MG, antibodies block, alter, or destroy these receptors, reducing the muscle's ability to contract and causing weakness.
Risk Factors
- Age: More common in women under 40 and men over 60.
- Sex: More common in women.
- Family history: Increased risk if there is a family history of autoimmune diseases.
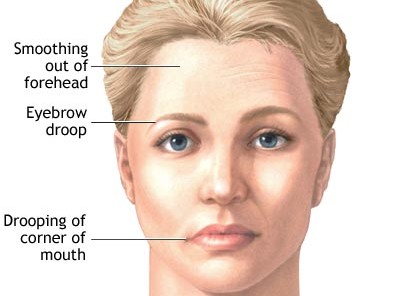
Signs and Symptoms
- Muscle weakness that worsens with activity and improves with rest.
- Ptosis (drooping of one or both eyelids).
- Diplopia (double vision).
- Difficulty swallowing (dysphagia) and chewing.
- Shortness of breath.
- Weakness in the arms, hands, fingers, legs, and neck.
Investigations
- Clinical history and physical examination, focusing on neurological and muscular assessment.
- Serological tests: Serum anti-acetylcholine receptor (ACh-R) antibody testing.
- Electromyography (EMG) and nerve conduction studies.
- Thyroid function test.
- Edrophonium test: Temporary improvement in muscle strength after administration of edrophonium chloride.
- Imaging: CT or MRI of the chest to check for thymomas.
- Pulmonary function tests: To assess respiratory muscle strength.
Management
Primary Care Management
- Initial assessment and referral to a neurologist for further evaluation and diagnosis.
- Supportive care, including managing symptoms and providing information and support to patients and families.
- Monitoring for complications, such as myasthenic crisis (severe muscle weakness leading to respiratory failure).
Example Management for Myasthenia Gravis
A patient presenting with symptoms of Myasthenia Gravis should be referred to a neurologist for a comprehensive evaluation. If diagnosed, the patient may be started on acetylcholinesterase inhibitors such as pyridostigmine to improve muscle strength. Immunosuppressive therapies may be considered to reduce the autoimmune response. The patient should receive multidisciplinary care, including physiotherapy to maintain muscle strength and regular follow-up to monitor disease progression and adjust the care plan as needed.
References
- NICE. (2024). Myasthenia Gravis: Management. Retrieved from NICE
- NHS. (2023). Myasthenia Gravis. Retrieved from NHS
- Howard, J. F., et al. (2018). Myasthenia Gravis: A Clinical Overview. Neurologic Clinics.
- Drachman, D. B. (1994). Myasthenia Gravis. New England Journal of Medicine.
- Conti-Fine, B. M., et al. (2006). Myasthenia Gravis: Past, Present, and Future. Journal of Clinical Investigation.
- Global Neurology Clinic Dubai (2019) *Myasthenia Gravis*. Available at: https://www.gncdubai.com/wp-content/uploads/2019/11/myasthenia-gravis.jpg (Accessed: 24 June 2024).
Check out our youtube channel
Blueprint Page
Explore the comprehensive blueprint for Physician Associates, covering all essential topics and resources.
Book Your Session
Enhance your skills with personalised tutoring sessions tailored for Physician Associates.



