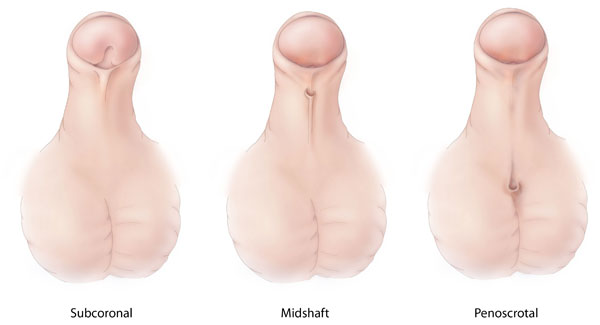
Image: "Hypospadias" by the Centers for Disease Control and Prevention (CDC) is licensed under CC0 (Creative Commons Zero). Link to the source.
Hypospadias in Children
Definition | Aetiology | Pathophysiology | Risk Factors | Signs and Symptoms | Investigations | Management | References
Definition
Hypospadias is a congenital condition in which the opening of the urethra (meatus) is located on the underside of the penis rather than at the tip. The condition can vary in severity depending on how far down the urethral opening is, ranging from just below the tip to the scrotum. In some cases, hypospadias is associated with chordee (a downward curvature of the penis) or other penile malformations.
Aetiology
Hypospadias results from incomplete development of the urethra during fetal development. The exact cause is often unknown, but factors that may contribute include:
- Genetic factors: a family history of hypospadias increases the risk.
- Hormonal factors: abnormal androgen levels or receptor function during fetal development can affect urethral formation.
- Environmental factors: exposure to certain chemicals, such as endocrine disruptors, during pregnancy may increase the risk of hypospadias.
- Maternal factors such as advanced maternal age or use of fertility treatments.
Pathophysiology
Hypospadias occurs when the urethral folds, which normally close to form the penile urethra during embryonic development, fail to close completely. As a result, the urethral opening remains on the underside of the penis. The severity of hypospadias depends on the position of the meatus along the penile shaft. In more severe cases, chordee (a downward curvature of the penis) may also occur, further complicating function and appearance.
Risk Factors
- Family history of hypospadias or other congenital urogenital abnormalities.
- Maternal exposure to certain endocrine-disrupting chemicals during pregnancy.
- Advanced maternal age.
- Use of fertility treatments such as in vitro fertilisation (IVF).
- Premature birth or low birth weight.
- Hormonal imbalances during fetal development, such as reduced androgen activity.
Signs and Symptoms
The presentation of hypospadias can vary based on the location of the urethral opening:
- Urethral opening located on the underside of the penis rather than at the tip.
- Abnormal urine stream direction, often downward or spraying.
- Curvature of the penis (chordee), particularly during erection.
- In severe cases, the scrotum may appear divided or the urethral opening may be located near the perineum.
- Difficulty with toilet training in older children due to abnormal urinary stream.
Investigations
Diagnosis of hypospadias is usually made based on clinical examination soon after birth. Further investigations may include:
- Physical examination: to assess the position of the urethral meatus, presence of chordee, and any associated penile anomalies.
- Ultrasound: may be used in some cases to assess the urinary tract for other associated abnormalities, particularly if the hypospadias is severe or other genital anomalies are present.
- Karyotyping: in cases of severe hypospadias with ambiguous genitalia, genetic testing may be performed to rule out intersex conditions.
Management
Treatment of hypospadias is surgical and aims to correct the position of the urethral opening, improve cosmetic appearance, and restore normal urinary and reproductive function.
Surgical Correction:
- Timing: surgery is typically performed between 6 and 18 months of age to correct the urethral opening and any associated chordee.
- Procedure: the surgeon will create a new urethral channel and reposition the urethral opening to the tip of the penis. In cases with chordee, the curvature will be corrected during the procedure.
- Multiple stages: in severe cases, surgery may be performed in multiple stages, particularly if there is significant penile curvature or complex reconstruction is needed.
Postoperative Care and Follow-up:
- Postoperative monitoring: after surgery, children are closely monitored for complications such as fistula formation (an abnormal connection between the urethra and the skin), strictures, or infection.
- Long term follow up: regular follow-up is necessary to ensure normal urinary and sexual function, particularly as the child grows and reaches puberty.
When to Refer:
- All cases of hypospadias should be referred to a paediatric urologist for assessment and surgical planning.
- Early referral is recommended, ideally in the first few months of life, to ensure timely intervention.
References
- NICE (2024). Hypospadias: Diagnosis and Management Guidelines. Available at: NICE Guidance
- BMJ (2023). Management of Hypospadias in Children. Available at: BMJ
- NHS (2023). Hypospadias in Infants. Available at: NHS
Check out our YouTube channel
Blueprint Page
Explore the comprehensive blueprint for Physician Associates, covering all essential topics and resources.
Book Your Session
Enhance your skills with personalised tutoring sessions tailored for Physician Associates.

