Ventricular Tachycardia
Definition | Aetiology | Pathophysiology | Risk Factors | Signs and Symptoms | Investigations | Management | Patient Advice
Definition
Ventricular Tachycardia (VT) is a life-threatening arrhythmia originating in the ventricles, characterised by a fast heart rate (≥100 beats per minute) with three or more consecutive ventricular beats. See Figure 1.
Aetiology
Causes of VT include:
- Ischaemic Heart Disease: Commonly occurs post-myocardial infarction due to scarring in the heart muscle.
- Cardiomyopathies: Conditions like dilated or hypertrophic cardiomyopathy.
- Electrolyte Abnormalities: Low potassium or magnesium levels.
- Drug Toxicity: E.g., digoxin toxicity or use of antiarrhythmics.
- Genetic Conditions: E.g., Long QT syndrome or Brugada syndrome.
Pathophysiology
VT occurs due to abnormal electrical activity in the ventricles:
- Re-entry Circuits: Electrical signals re-enter damaged areas, causing repetitive ventricular activation.
- Enhanced Automaticity: Increased spontaneous electrical activity in ventricular cells.
- Trigger Activity: Abnormal electrical signals triggered by afterdepolarisations.
Risk Factors
Factors increasing the risk of VT include:
- Previous myocardial infarction.
- Heart failure or reduced left ventricular ejection fraction (LVEF).
- Electrolyte disturbances, e.g., low potassium or magnesium.
- Family history of genetic arrhythmia syndromes.
- Use of QT-prolonging medications.
Signs and Symptoms
Symptoms of VT include:
- Palpitations: Sensation of rapid or irregular heartbeats.
- Dizziness: Caused by reduced cardiac output.
- Syncope: Sudden loss of consciousness due to inadequate blood flow to the brain.
- Chest Pain: Due to reduced oxygen supply to the heart muscle.
- Shortness of Breath: Due to decreased cardiac efficiency.
Investigations
Tests to diagnose VT include:
- 12-Lead ECG:
- Shows wide QRS complexes (>120 ms) and a fast ventricular rate.
- Fusion or capture beats may indicate VT rather than supraventricular tachycardia (SVT).
- Blood Tests:
- Electrolytes: Check potassium, magnesium, and calcium levels.
- Cardiac Markers: Elevated troponins may indicate myocardial ischaemia.
- Echocardiography: Assesses ventricular function and identifies structural abnormalities.
- Cardiac MRI: Evaluates scarring or fibrosis in the myocardium.
- Electrophysiological Study (EPS): Maps abnormal electrical pathways and identifies re-entry circuits.
Management
1. Acute Management
- Unstable VT: Immediate synchronised electrical cardioversion.
- Stable VT: Antiarrhythmic medications such as amiodarone (300 mg IV loading dose, then 900 mg over 24 hours).
2. Long-Term Management
- Implantable Cardioverter-Defibrillator (ICD): Device implanted to detect and treat VT episodes automatically.
- Catheter Ablation: Procedure to destroy re-entry circuits in cases of recurrent or refractory VT.
- Medication: Beta-blockers (e.g., bisoprolol) or antiarrhythmics (e.g., sotalol) to prevent recurrences.
3. Specialist Referral
Referral to cardiology is essential for:
- Assessment for ICD implantation.
- Evaluation for underlying causes, including ischaemia or cardiomyopathy.
Patient Advice
Key advice includes:
- Avoid triggers such as stress, stimulants, and QT-prolonging medications.
- Take medications as prescribed to prevent recurrence.
- Maintain regular follow-up appointments to monitor heart health and device function if an ICD is implanted.
- Seek urgent medical attention if symptoms like chest pain, syncope, or palpitations recur.
Figure 1
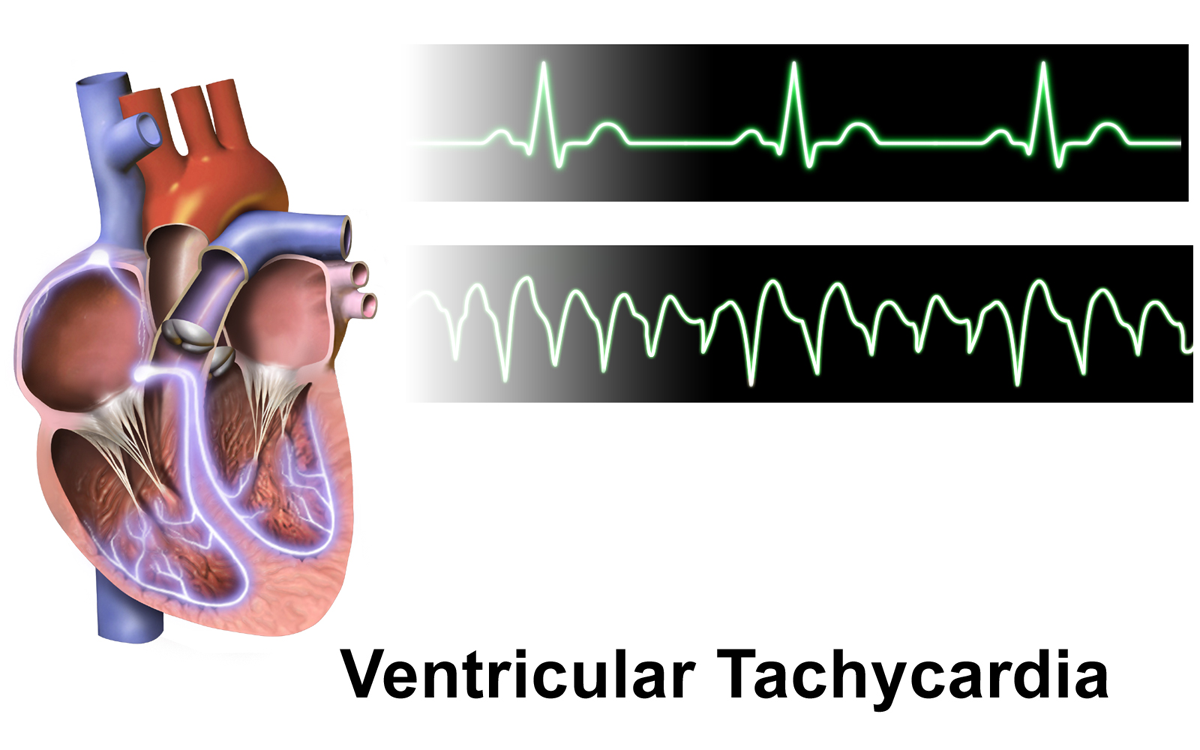
Image showing an ECG example of ventricular tachycardia.
References
- BruceBlaus (2015). Ventricular Tachycardia [Image]. Available at: https://upload.wikimedia.org/wikipedia/commons/d/d4/Ventricular_Tachycardia.png (Accessed: 30 December 2024).
